
Module 10: Navigating challenges during rehabilitation

Navigating Challenges
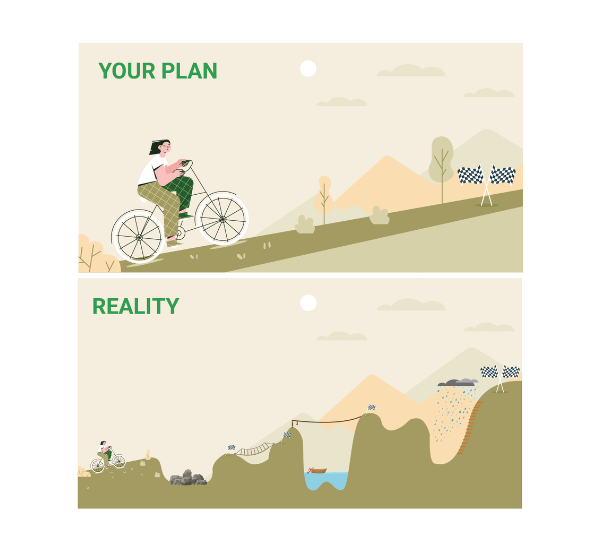
As you move through your rehab journey, there will be challenges along the way. You might remember this image from Module 5: What does recovery look like?
Going through rehab is very similar to driving on an uphill road. You might be expecting a smooth and steady drive to the top. But along the way, you notice that the road goes up and down. It can stay flat for a long time followed by sudden twists and sharp turns. The ride might be fun for some parts and boring at others. You might want to turn around and go home at some points. Then eventually you reach your destination.
Many drivers find it helpful to look at a map before going on a trip. This helps them to prepare for any difficult sections over rough terrain. Having realistic expectations of the road ahead can help you to keep going through the difficult moments.
This module will help you to understand some of the challenges you might face through rehab – and give you some tips and tricks to work through these difficult moments.
You will find it hard to pay attention
Most people find that their attention is worse after brain injury. This happens for people with mild, moderate and severe TBI (1). You might have trouble with one or more types of attention including visual (i.e. taking in imagery and objects around you), spatial (i.e. directing your attention to a location in space), or auditory (i.e. taking in important sounds and filtering out background noise).
Many people find it hard to do their rehab exercises when they have poor attention. Attention problems often cause feelings of frustration and hopelessness during rehab (2). You might want to give up because it feels like there’s there is no point in doing rehab – this is really common for people with TBI.
Doing as much as you can counts for a lot – whether it’s 10 seconds, 1 minute or 10 minutes. Each time you do an exercise, your brain creates new structures and pathways to replace the ones damaged during your injury. Over time, with practice and training, many people with a TBI are able to improve their attention (2).
New symptoms might appear
It’s common for people with TBI to report new symptoms or difficulties months or years after injury (3). These new symptoms or difficulties which appear at a later time are called late effects or delayed effects (4). It can be scary when new symptoms suddenly appear. Some people think this means their TBI is getting worse – but this isn’t true. Late or delayed symptoms are caused by changes in the brain which occurred at the time of injury – they just take a long time to become noticeable (4).
It can be frustrating or discouraging to have to deal with new or changing symptoms. You might feel like you’re going backwards or starting again with your rehab whenever a new symptom appears. It’s important to recognise that this is a normal part of brain injury recovery (3).
It’s important to report any new symptoms to your rehab team as soon as you notice them. Your team will be able to modify your rehab exercises and help you work on any new areas.
Your energy levels will go up and down
Fatigue is very common after TBI. It’s estimated that around 80% of people with a TBI have problems with fatigue which can last for as many as five years after injury (5).
Normal fatigue is a conscious decrease in a person’s ability to perform physical or mental tasks or activities (6). It’s often described as a feeling of physical or mental weariness that occurs after a period of activity or exertion (7).
For example, you might feel physically fatigued after a few rounds of strength and conditioning exercises with your physio. This is caused by muscle exertion. Or you might feel mentally fatigued after doing some communication exercises with your speech therapist. You can feel physically and mentally fatigued at the same time.
With a TBI, you will find that you become fatigued faster and more easily after doing activities (7). Let your therapists know whenever you need a break.
Sometimes you may feel fatigued even if you have not done any activities, and the fatigue may not disappear after rest. This is called pathological fatigue and is caused by changes in the brain and body after injury (7). This type of fatigue is more intense and prolonged than normal fatigue (8), can be difficult to treat and can interfere with your rehab.
Sometimes, fatigue and low energy levels can be caused by sleep problems. Over 50% of people with a TBI experience some form of sleep disturbance (9). There are behavioural treatments or medications to help with sleep problems. Your rehab team can liaise with your doctor to prescribe any medications if needed.
Your motivation will go up and down too
Motivation is important in determining the outcome of rehabilitation (10). Generally, people who have higher motivation show larger improvements at the end of rehab compared to those with lower motivation (11). Researchers believe this happens as people who have higher motivation are more likely to actively participate (or try their best) in rehab. They are then more likely to make progress – which in turn boosts their motivation (12). This is called a positive feedback loop (13).
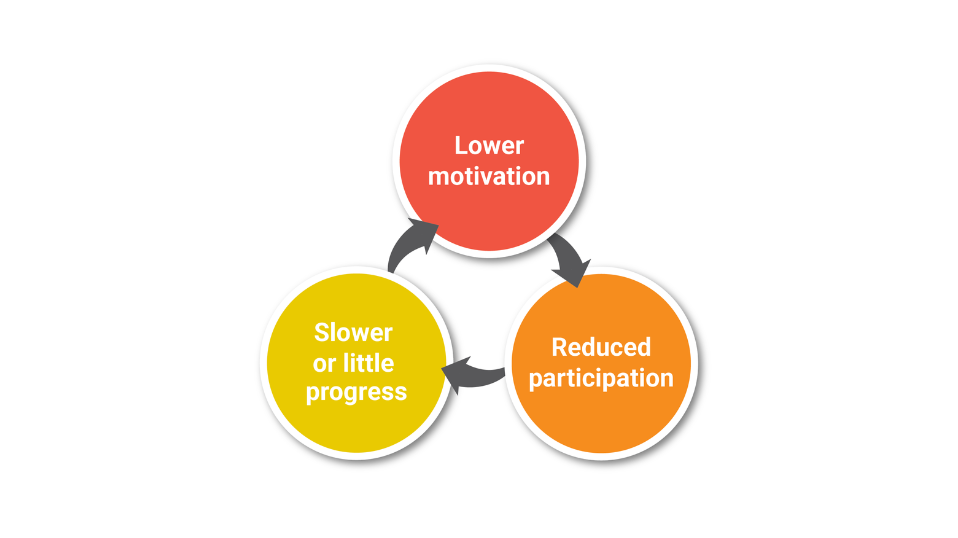
The opposite happens when a person has low motivation. People with lower motivation are less likely to try their best during rehab. This causes them to show slower or little progress – which in turn reduces their motivation. This is called a negative feedback loop. So as you can see, motivation is really important.
But it’s not realistic to be highly motivated throughout your whole rehab journey. Most people find that their motivation goes up and down. This is normal.
When you’re feeling unmotivated, the trick is to try not to stay in the low motivation zone for too long – or you might get stuck in the negative feedback loop.
Here are some ways to increase your motivation when you’re just not feeling it:
- Start small – commit to doing the first 2 minutes of your rehab session. If you want you can stop after that. Sometimes getting started is the hardest part. Once you have started, you might find that you’re more motivated to continue. This is called behavioural activation (14).
- Change your environment – ask your therapist if you can do some sessions outside or in a different setting. Have a different playlist for each session. These small setting changes can break the routine and repetitiveness of rehab.
- Reward yourself for your hard work,
- Try positive self-talk (e.g. “I am getting stronger every day”, “What I choose to do today will help get me closer to my goals”),
- Talk to someone about why you’re feeling unmotivated.

Other possible challenges during rehabilitation
There may be other challenges that come your way during rehab. A typical rehab program can take 1-2 years to complete so there can be lots of changes that happen along the way. Some possible challenges include:
- You might feel bored,
- You might feel that your progress is slower than expected,
- Your goals might change,
- You might compare your progress with that of your peers,
- You might not get along with all of your therapists or peers,
- Your therapists might change,
- You might need to changes services.
Your rehabilitation coordinator or case coordinator will be an important person throughout your rehab journey. They will communicate with you about any changes to your team, services or funding.
It’s also important for you to communicate with your rehabilitation coordinator if you’re having any issues with any part of your program, team or peers. They will be able to support you to find
References
- Lee HY, Hyun SE, Oh B-M. Rehabilitation for Impaired Attention in the Acute and Post-Acute Phase After Traumatic Brain Injury: A Narrative Review. Korean journal of neurotrauma. 2023;19(1):20.
- Michel J, Mateer C. Attention rehabilitation following stroke and traumatic brain injury. Europa medicophysica. 2006;42(1):59-67.
- Feuston JL, Marshall-Fricker CG, Piper AM, editors. The social lives of individuals with traumatic brain injury. Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems; 2017.
- Gualtieri CT. Delayed neurobehavioral sequelae of traumatic brain injury. Neuropsychiatry and Behavioral Pharmacology. 1991:26-36.
- Olver JH, Ponsford JL, Curran CA. Outcome following traumatic brain injury: a comparison between 2 and 5 years after injury. Brain injury. 1996;10(11):841-8.
- Aaronson LS, Teel CS, Cassmeyer V, Neuberger GB, Pallikkathayil L, Pierce J, et al. Defining and measuring fatigue. Image: the journal of nursing scholarship. 1999;31(1):45-50.
- Belmont A, Agar N, Hugeron C, Gallais B, Azouvi P, editors. Fatigue and traumatic brain injury. Annales de réadaptation et de médecine physique; 2006: Elsevier.
- Jason LA, Evans M, Brown M, Porter N. What is fatigue? Pathological and nonpathological fatigue. PM&R. 2010;2(5):327-31.
- Rao V, Spiro J, Vaishnavi S, Rastogi P, Mielke M, Noll K, et al. Prevalence and types of sleep disturbances acutely after traumatic brain injury. Brain injury. 2008;22(5):381-6.
- Maclean N, Pound P, Wolfe C, Rudd A. A critical review of the concept of patient motivation in the literature on physical rehabilitation. Soc Sci Med. 2000;50(4):495-506.
- Maclean N, Pound P, Wolfe C, Rudd A. Qualitative analysis of stroke patients' motivation for rehabilitation. Bmj. 2000;321(7268):1051-4.
- Martin R, Levack WM, Sinnott KA. Life goals and social identity in people with severe acquired brain injury: an interpretative phenomenological analysis. Disability and Rehabilitation. 2015;37(14):1234-41.
- Krau E. Motivational feedback loops in the structure of action. Journal of Personality and Social Psychology. 1982;43(5):1030.
- Veale D. Behavioural activation for depression. Advances in Psychiatric Treatment. 2008;14(1):29-36.